Klinisk Biokemi i Norden · 2 2017
| 11
profile is conventionally measured in blood plasma or
serum obtained after fasting for at least 8 hours, and
therefore may not reflect the daily average plasma lipid
and lipoprotein concentrations and associated risk of
cardiovascular disease
3,4
.
Interestingly, evidence is lacking that fasting is supe-
rior to nonfasting when evaluationg the lipid profile
for cardiovascular risk assessment. However, there are
advantages to using nonfasting samples rather than
fasting samples for measuring the lipid profile
5-9
. Since
2009, nonfasting lipid testing has become the clinical
standard in Denmark, based on recommendations
from the Danish Society for Clinical Biochemistry that
all laboratories in Denmark use random nonfasting
lipid profiles as the standard, while offering clinicians
the option of re-measuring triglyceride concentra-
tions in the fasting state if nonfasting values are >4
mmol/L(350mg/dL)
10,11
. Furthermore, the UK NICE
guidelines have endorsed nonfasting lipid testing in
the primary prevention setting since 2014
12
. Since
publication of our consensus paper, nonfasting lipid
profiles has also been introduced as the standard in
Canada and Brazil.
The most obvious advantage of nonfasting rather
than fasting lipid measurements is that it simplifies
blood sampling for patients, laboratories, general
practitioners, and hospital clinicians and is also likely
to improve patient compliance with lipid testing
5-9
.
Indeed, patients are often inconvenienced by having to
return on a separate visit for a fasting lipid profile and
may default on essential testing. Also, laboratories are
burdened by a large volume of patients attending for
tests in the morning. Finally, clinicians are burdened
by having to review and make decisions on the fin-
dings in the lipid profile at a later date. This situation
may also require an additional phone call, e-mail, or
even a follow-up clinic visit, placing extra workloads
on busy clinical staff.
Perceived limitations to adopting nonfasting lipid
measurements include: 1) Fasting before a lipid profile
measurement is believed to provide more standardized
measurements; 2) Nonfasting lipid profiles are percei-
ved as providing less accurate measurements and may
make calculation of LDL cholesterol via the Friedewald
equation invalid; 3) As fasting has been the clinical
standard, it is unclear what values should be flagged
as abnormal when using nonfasting rather than fasting
plasma lipid profiles. These perceived limitations will
be addressed in this paper.
The aims of the present joint consensus statement
are to critically evaluate the use of nonfasting rather
than fasting lipid profiles, and the clinical implications
of this question with a view to providing appropriate
guidance for laboratory and clinicians. Based on evi-
dence from large-scale population studies and regist-
ries and on consensus of expert opinions, the EAS/
EFLM joint consensus statement proposes recommen-
dations on (i) situations when fasting is not required for
a lipid profile, and (ii) on how laboratory reports should
flag abnormal lipid profiles to improve compliance of
patients and clinicians with concentration goals used
in guidelines and consensus statements on cardiovas-
cular disease prevention
13-17
. Key recommendations
are given in Table 1.
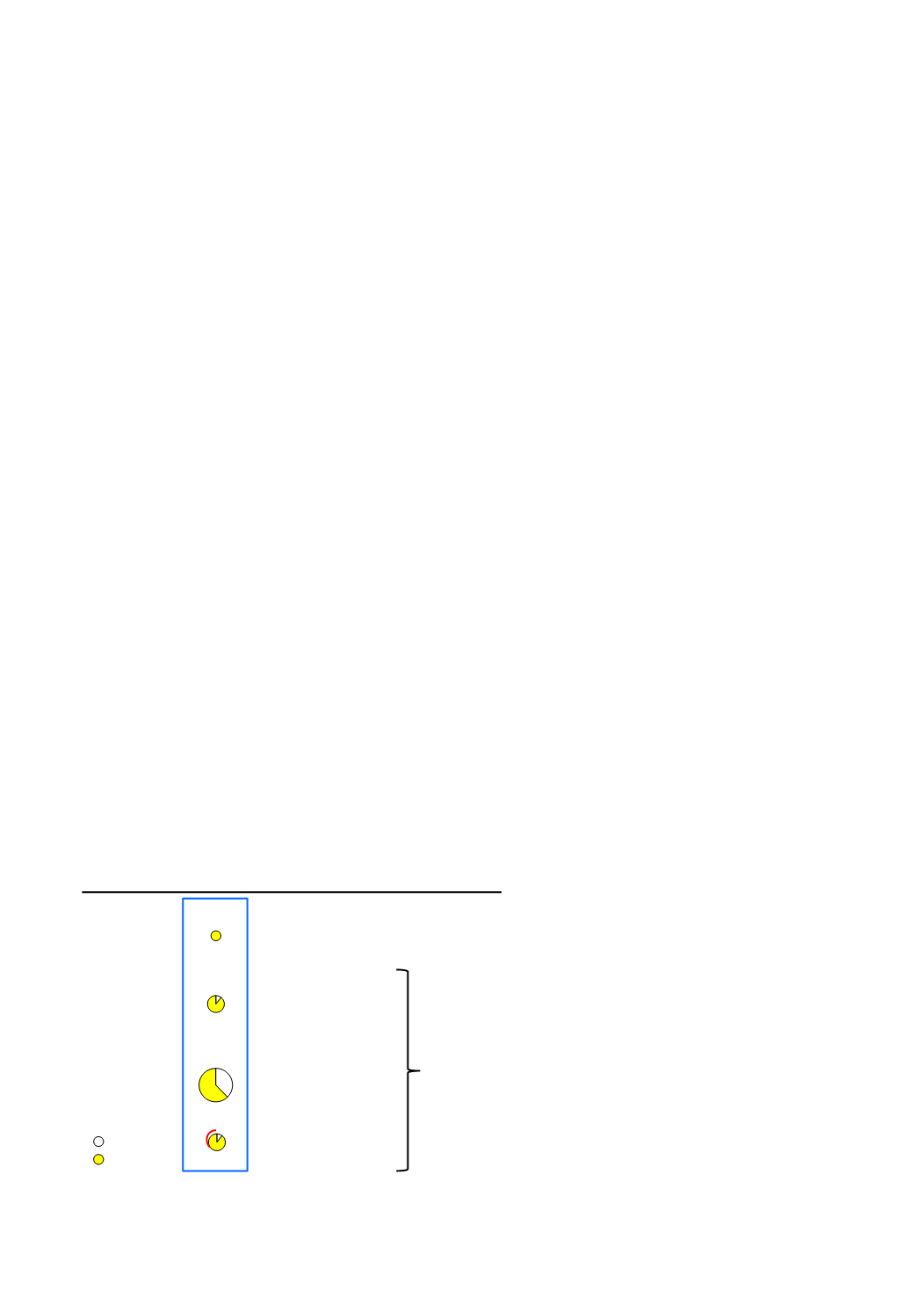
Figure 1. Lipids, lipoproteins and apolipoproteins as
part of standard and expanded lipid profiles. Standard
lipid profiles consist of triglycerides and total, LDL,
and HDL cholesterol; however, a standard lipid profile
could also report calculated remnant cholesterol and
calculated nonHDL cholesterol as these come at no
additional cost. Calculated remnant cholesterol is non-
fasting total cholesterol minus LDL cholesterol minus
HDL cholesterol. Calculated nonHDL cholesterol is
total cholesterol minus HDL cholesterol. Lipoprotein(a)
should be measured at least once in every individual
screened for cardiovascular risk in order to detect
potentially high concentrations of this genetic risk
factor. Finally, apolipoprotein B and apolipoprotein A1
can be used as alternatives to nonHDL and HDL cho-
lesterol, but these measurements come at an extra cost.
Figure designed by Prof B. G. Nordestgaard.
Apo A1
Triglycerides
Cholesterol
HDL
Remnants
LDL
Lipoproteins
HDL cholesterol
Remnant cholesterol
LDL cholesterol
ApoB
or
non-HDL
cholesterol
Alternative
Triglycerides
Lipids
Lp(a) total mass
Lp(a)
Figure 1